Status Epilepticus Management Guide for 2025
Introduction
Status epilepticus (SE) is a neurological emergency characterized by prolonged or recurrent seizures without full recovery of consciousness between episodes. It is defined as a seizure lasting more than 5 minutes or two or more seizures without regaining baseline consciousness. SE requires urgent medical intervention to prevent severe complications such as brain damage, respiratory failure, and death.
What is the Best Approach to Managing Status Epilepticus?
Effective management of SE requires rapid diagnosis and a structured treatment approach. This guide outlines essential steps based on the latest clinical guidelines, helping healthcare providers act swiftly to reduce morbidity and mortality.
1. Recognizing Status Epilepticus
- SE is defined as continuous seizure activity lasting >5 minutes or recurrent seizures without full recovery.
- It can present as:
- Convulsive SE: Generalized tonic-clonic seizures
- Non-convulsive SE: Altered consciousness without visible convulsions
- Focal SE: Persistent focal motor seizures
- Early recognition is critical to prevent irreversible brain damage.
2. Common Causes of Status Epilepticus
- Missed Antiepileptic Drugs (AEDs) in known epileptic patients (most common)
- Metabolic disturbances (hypoglycemia, hyponatremia, hypoxia, etc.)
- Structural brain injuries (stroke, tumor, head trauma)
- CNS infections (meningitis, encephalitis)
- Toxic/Drug-induced SE (alcohol withdrawal, overdoses, poisoning)
- Autoimmune or unknown causes
3. Diagnosis: Clinical and EEG Confirmation
- Clinical diagnosis is based on seizure activity and altered consciousness.
- EEG (if available) is useful, especially for non-convulsive SE.
- Blood tests: Glucose, electrolytes, renal function, toxicology, and arterial blood gases.
- Neuroimaging (CT/MRI) if structural cause is suspected.
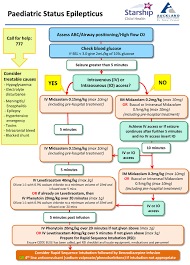
4. Immediate Treatment: First 30 Minutes are Crucial
Step 1: Initial Emergency Management
- Airway, Breathing, Circulation (ABC)
- IV Access & Monitoring: Cardiac monitoring, oxygen support, IV fluids
- Labs: Blood glucose, electrolytes, renal function, and arterial blood gases
- Correct Metabolic Causes: Administer
- IV Glucose (for hypoglycemia)
- IV Thiamine (for alcohol-related seizures)
- IV Naloxone (if opioid overdose suspected)
Step 2: First-Line Medications (0-5 minutes)
- Benzodiazepines are first-line therapy:
- IV Lorazepam (0.1 mg/kg, max 4 mg, repeat in 10-15 min if needed)
- If IV not available: IM Midazolam (0.2 mg/kg) or Rectal Diazepam (0.5 mg/kg)
Step 3: Second-Line Medications (5-20 minutes, if seizures persist)
- Administer an IV antiepileptic drug (AED):
- Phenytoin/Fosphenytoin (20 mg/kg IV at 50 mg/min)
- Levetiracetam (60 mg/kg IV, max 4500 mg)
- Valproic Acid (40 mg/kg IV, max 3000 mg)
Step 4: Third-Line Treatment (20-40 minutes, if seizures persist)
- Repeat AED loading dose (usually half of initial dose)
- Consider ICU admission and preparation for anesthesia if seizures are ongoing
Step 5: Refractory Status Epilepticus (40+ minutes, if seizures continue)
- Intubate & Start General Anesthesia using:
- Midazolam Infusion (0.1 mg/kg/hr)
- Propofol Infusion (1-2 mg/kg bolus, then 5-10 mg/kg/hr infusion)
- Phenobarbital (20 mg/kg IV)
- Continuous EEG monitoring is recommended.
5. Post-Seizure Management and Long-Term Care
- Restart regular AEDs and adjust doses if needed.
- Identify and treat underlying causes (infection, metabolic imbalance, structural lesions).
- Prevent complications: Aspiration pneumonia, rhabdomyolysis, acidosis, and hypoxia.
- Patient and family counseling on epilepsy management and drug adheren
Conclusion
Status Epilepticus is a medical emergency requiring immediate recognition and treatment. Benzodiazepines are the first-line therapy, followed by AEDs, and if seizures persist, ICU management with general anesthesia is necessary. Early intervention significantly reduces the risk of neurological damage and mortality.
Timely management, proper diagnostics, and preventive strategies can improve patient outcomes and reduce recurrence risks. If you suspect SE, act FAST and follow the structured ABCDE approach outlined in this guide.
Ultimate guide to Managing Status Epilepticus
Complications of Status Epilepticus
Status epilepticus (SE) can lead to serious complications, including:
- Neurological Damage – Prolonged seizures cause excitotoxicity, leading to neuronal injury and brain damage.
- Cognitive Impairment – Memory loss, attention deficits, and long-term cognitive decline can occur.
- Hypoxia and Respiratory Failure – Seizures can impair breathing, leading to hypoxia, acidosis, and potential respiratory arrest.
- Cardiovascular Complications – Arrhythmias, hypertension, hypotension, and even cardiac arrest may result from autonomic instability.
- Rhabdomyolysis and Acute Kidney Injury – Prolonged muscle contractions can cause muscle breakdown, leading to renal failure.
- Metabolic Disturbances – Lactic acidosis, hyperkalemia, and electrolyte imbalances may occur due to prolonged seizure activity.
- Aspiration Pneumonia – Impaired airway reflexes increase the risk of aspiration and subsequent pneumonia.
- Increased Mortality Risk – If untreated, SE has a high fatality rate, particularly in refractory cases.
