A 38-year-old pregnant woman, at 8 months of gestation, presented with gastric pain. She was initially evaluated at a local hospital, where investigations revealed a hemoglobin level of 6 g/dL. She was promptly transfused with 1500 cc of blood. Three days later, she developed left-sided hemiparesis, generalized seizures, and loss of consciousness. At this point, she was in a remote village with limited medical facilities. After a 3-day transport, she arrived at our hospital.
Upon admission, a thorough physical examination was conducted. The patient presented with generalized seizures, left-sided hemiparesis, and lower limb edema. Her vital signs were stable, and her blood pressure was within normal limits. However, the patient was in a coma, with a Glasgow Coma Scale (GCS) score below 8.
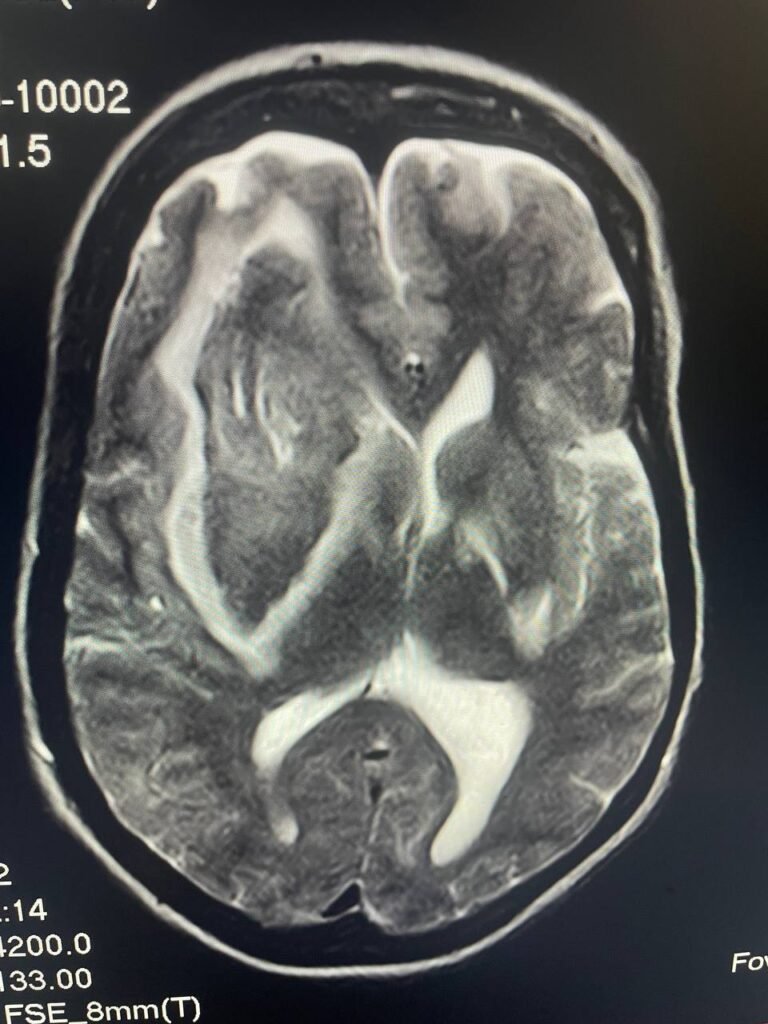
Given her pregnancy, we opted for an MRI scan instead of a CT scan, as CT is contraindicated in pregnant patients. MRI results, obtained one hour later, revealed a significant intracranial hemorrhage in the right hemisphere.

Medical Insights:
- Pregnancy and Hemorrhage: Intracranial hemorrhages during pregnancy, though rare, can be life-threatening for both the mother and fetus. Immediate and careful diagnosis and management are critical to improve outcomes.
- MRI vs. CT in Pregnancy: When imaging is needed in pregnant patients, MRI is the preferred method due to its safety profile compared to CT, which uses ionizing radiation.
- Hemoglobin Levels and Complications: The patient’s initial low hemoglobin (6 g/dL) could have contributed to the development of further complications. Iron deficiency anemia in pregnancy is common but must be managed appropriately to prevent adverse outcomes like seizures and intracranial events.
Conclusion
This case underscores the importance of early identification and management of potentially life-threatening conditions, especially in pregnant patients. The use of MRI in this scenario allowed for a safe and accurate diagnosis of intracranial hemorrhage, enabling timely intervention.
4 Responses
[…] Abstract […]
[…] Case: Subacute And Subgaleal Hematoma After Head Trauma In 16-Year-Old Boy on Intracranial Hemorrhage in a Pregnant WomanAugust 5, […]
I will right away grab your rss as I can not in finding your e-mail subscription hyperlink or newsletter service. Do you’ve any? Please let me recognize in order that I could subscribe. Thanks.
You can follow our latest posts using the RSS feed. Email subscription support may be added in the future, Thank you