Introduction
Headaches and neck pain are common symptoms in elderly patients, but when accompanied by limb weakness, vomiting, and general malaise, they warrant serious attention. This case presents a 74-year-old patient diagnosed with bilateral chronic subdural hematomas with acute hemorrhagic components. After MRI confirmation of significant mass effect and a midline shift, urgent neurosurgical intervention became the only viable management option.
Case Presentation
Patient Background and Initial Complaint
A 74-year-old male patient presented to the outpatient department with a complaint of persistent headache, neck pain, and general malaise over the past few weeks. Over the preceding five days, the symptoms had escalated. The patient started experiencing intermittent vomiting, progressive weakness in both upper and lower limbs, and difficulty in ambulation. There was no recent history of trauma, seizures, or loss of consciousness.
The patient’s family reported increased drowsiness, poor appetite, and reduced responsiveness in conversation, particularly in the last two days. His past medical history included hypertension and type 2 diabetes mellitus, both moderately controlled with medication.
Physical Examination
On clinical examination:
- The patient was alert but slightly confused (GCS 13/15).
- Vital signs: BP 160/92 mmHg, HR 82 bpm, Temp 36.8°C.
- Neurological examination revealed:
- Weakness (Grade 3/5) in both upper and lower limbs.
- Hyperreflexia on both sides.
- Positive Babinski reflex bilaterally.
- Neck stiffness without photophobia.
- No papilledema was observed during fundoscopy.
Given the alarming symptoms in an elderly individual, we suspected an intracranial pathology and immediately ordered further diagnostic imaging
Radiological Findings
Bilateral Chronic Subdural Hematoma
MRI Brain Report
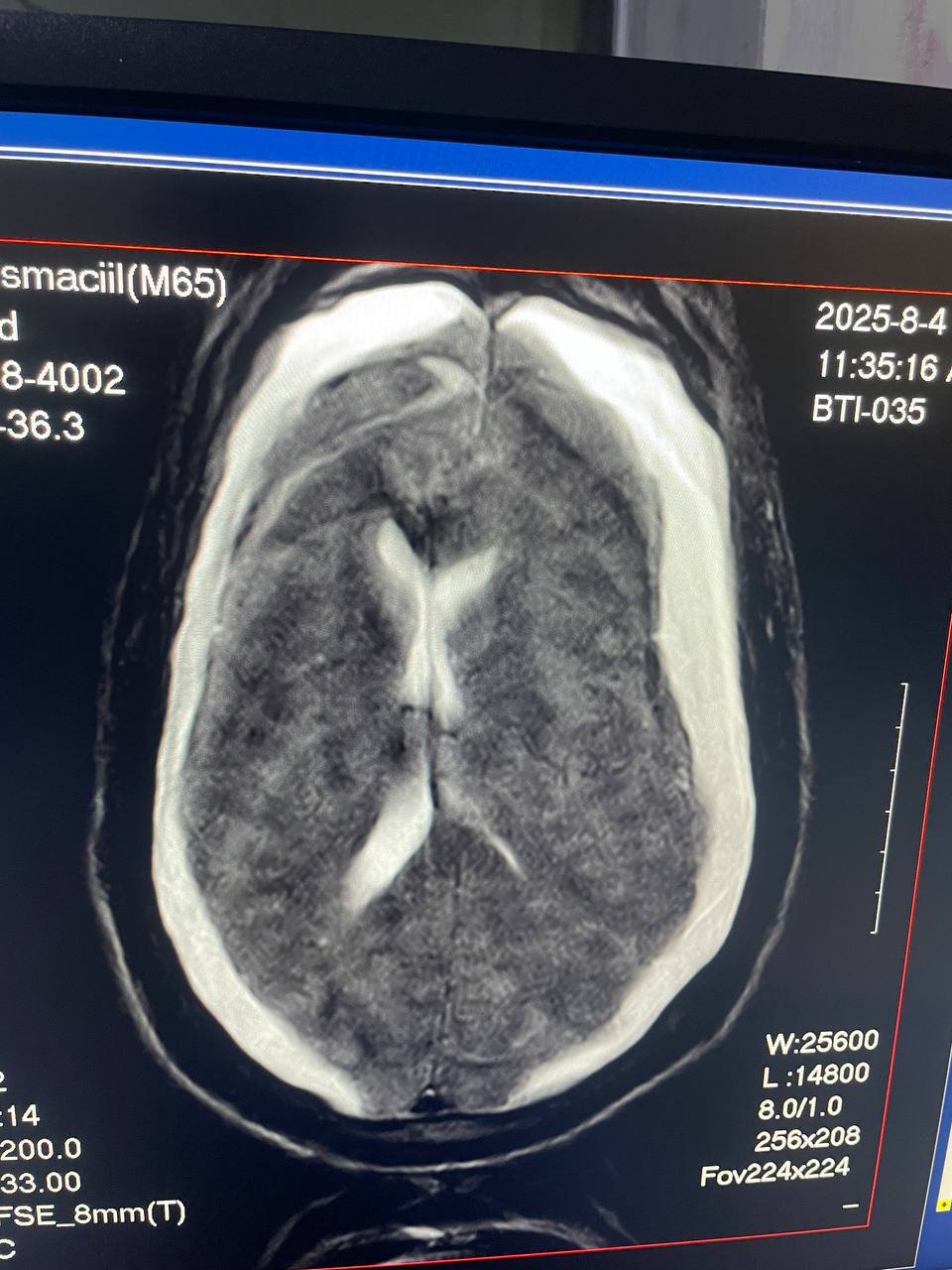
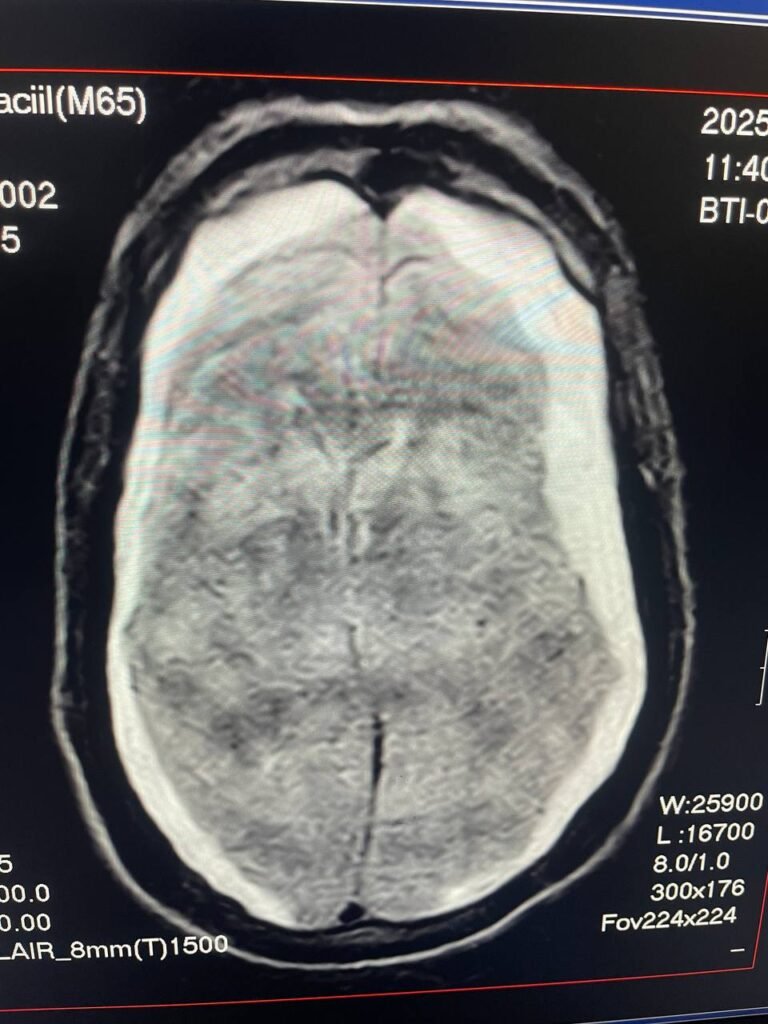
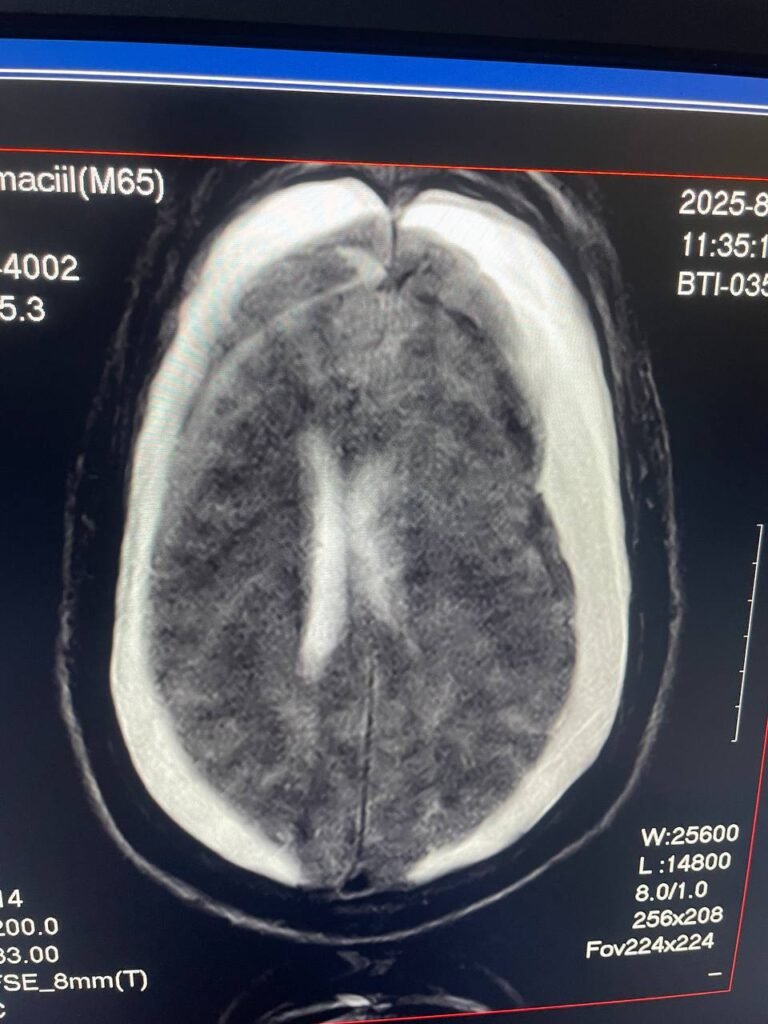
A contrast-enhanced MRI brain was performed, revealing the following:
Chronic subdural hematoma (SDH) with minimal acute hemorrhage involving: Bilateral frontal, parietal, temporal, and occipital regions.
Maximum thickness:
- 2.6 cm on the left side.
- 1.9 cm on the right side.
Mass effect on underlying brain tissue and lateral ventricles.
Midline shift of 9.9 mm toward the right side.
These findings confirmed the diagnosis of acute on chronic bilateral subdural hematomas with significant pressure effects on the brain.
Diagnosis
Based on clinical findings and MRI results, the patient was diagnosed with:
Acute on chronic bilateral subdural hematomas
with significant midline shift and neurological deficits.
Discussion
Understanding Chronic Subdural Hematoma in the Elderly
Chronic subdural hematoma (CSDH) is a relatively common neurosurgical condition in elderly individuals. Due to cerebral atrophy with aging, the bridging veins are more prone to shearing, even with minor or unnoticed head trauma.
In some patients, the slow venous bleeding leads to gradual collection of blood in the subdural space. Over time, it may become organized and encapsulated by membranes. Re-bleeding can occur spontaneously or with minor trauma, converting the hematoma into an acute on chronic type — often seen in this case.
Symptoms and Neurological Impact
Symptoms vary from subtle cognitive changes to significant neurological deterioration. In this case, the patient presented with:
- Persistent headache (due to increased intracranial pressure).
- Vomiting (suggesting raised ICP).
- Weakness in limbs (indicating cortical compression).
- Confusion and reduced consciousness.
These are hallmark features of progressive mass effect and brain shift.
Indications for Surgery
While some chronic SDH cases can be managed conservatively with steroids or close monitoring, this case clearly did not fall into that category. The decision for surgical intervention was made based on:
- Hematoma thickness (>2 cm on left, >1.5 cm on right
- Significant midline shift (9.9 mm)
- Worsening neurological signs
- Symptoms of raised intracranial pressure
These are absolute indications for evacuation to prevent herniation and irreversible damage.
Differential Diagnosis Considered
Initially, several possibilities were considered before imaging:
- Subarachnoid hemorrhage
- Meningitis (due to neck stiffness and malaise)
- Ischemic stroke
- Brain tumor or space-occupying lesion
However, MRI confirmed the hematoma diagnosis definitively.
Management Plan
Neurosurgical Intervention
After neurologist and neurosurgical consultation, the patient was transferred to the operating room. The chosen procedure was:
Bilateral burr-hole evacuation of the subdural hematoma under general anesthesia.
Intraoperatively:
- Dark fluid hematoma was evacuated.
- Hemostasis achieved.
- Subdural drains were placed bilaterally.
Postoperative Course
The patient was monitored in the ICU for 48 hours with:
- Frequent neurological assessments
- Head elevation
- Antiepileptic prophylaxis
- Strict blood pressure control
He showed significant improvement in mental status by day 3 post-operation. Limb strength also began to recover gradually.
Outcome and Follow-Up
After one week, the patient’s condition improved remarkably:
- Headache resolved.
- Limb strength improved to Grade 4/5.
- Orientation returned to normal
He was discharged on day 10 with physiotherapy and follow-up MRI scheduled in 4 weeks.
Conclusion
This case demonstrates the importance of early recognition and imaging in elderly patients presenting with neurological complaints. While conservative management may be suitable for some chronic SDHs, acute-on-chronic bilateral subdural hematomas with midline shift demand urgent surgical intervention.
Timely MRI scanning, accurate diagnosis, and prompt surgery played a life-saving role in this patient’s recovery. Delay in treatment could have led to catastrophic outcomes such as brain herniation, coma, or death.
One response
[…] Bilateral Chronic Subdural Hematoma Elderly on Intracranial Hemorrhage in a Pregnant WomanAugust 7, 2025 […]