Introduction
Cerebral edema, or brain swelling, is a critical medical condition where excess fluid accumulates in the brain, leading to increased intracranial pressure (ICP). This pressure can compromise brain function and, if untreated, may result in severe neurological damage or death. Understanding the underlying causes, recognizing early symptoms, and knowing the available treatment options are essential for effective management.
What Is Cerebral Edema?
Cerebral edema refers to the swelling of the brain due to an accumulation of excess fluid. This condition can disrupt normal brain function by increasing intracranial pressure, reducing cerebral blood flow, and potentially leading to brain herniation. It is always secondary to an underlying disease and isn’t a primary diagnosis.
Causes of Cerebral Edema
Cerebral oedema can result from various conditions, broadly categorized into:
1. Vasogenic Oedema
Occurs when the blood-brain barrier is disrupted, allowing proteins and fluids to leak into the extracellular space. Common causes include:
- Brain tumors
- Infections
- Trauma
- Radiation
2. Cytotoxic Oedema
Results from cellular injury leading to the failure of ion pumps, causing cells to swell. This type is often seen in:
- Ischemic stroke
- Hypoxia
- Hypoglycemia
3. Osmotic Oedema
Occurs when there is an imbalance in osmotic forces, leading to water influx into cells. Causes include:
- Hyponatremia
- Hyperglycemia
- Rapid correction of hyperglycemia
4. Hydrostatic (CSF Seepage) Oedema
Caused by increased cerebrospinal fluid pressure, leading to fluid leakage into brain tissue. Associated with conditions like:
- Hydrocephalus
- Meningitis
- Subarachnoid hemorrhage
Symptoms of Cerebral Oedema
The clinical manifestations of cerebral oedema depend on the severity and location of the swelling. Common symptoms include:
- Headache
- Nausea and vomiting
- Altered consciousness
- Seizures
- Focal neurological deficits
- Papilledema
- Cushing’s triad (hypertension, bradycardia, irregular respirations)
Early detection is crucial, as symptoms may be subtle in the initial stages.
Diagnosis
Diagnosing cerebral oedema involves a combination of clinical evaluation and imaging studies:
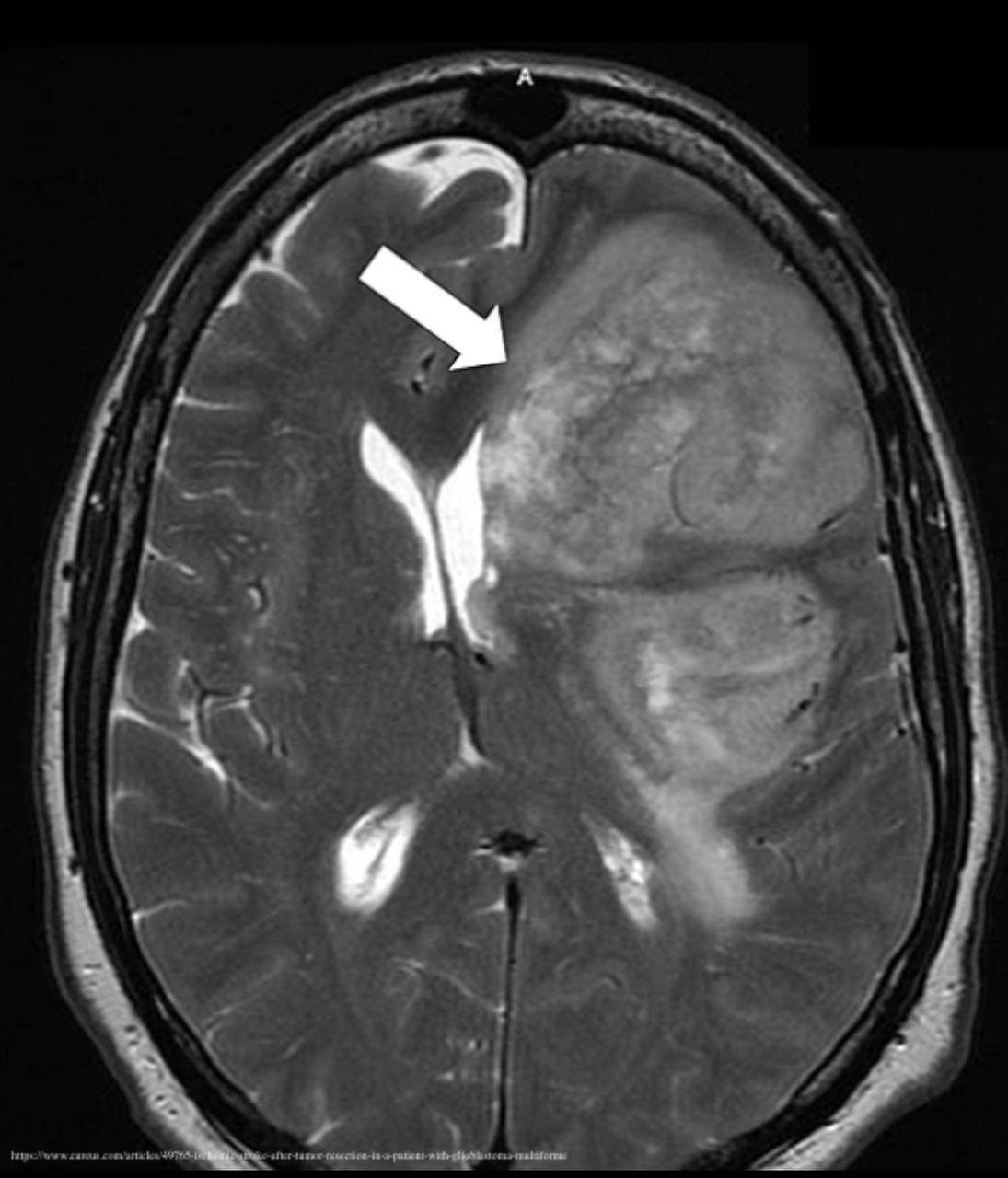
- CT Scan: Useful in detecting early signs of oedema, such as loss of gray-white matter differentiation and compression of ventricles.
- MRI: Provides detailed images; T2-weighted and FLAIR sequences are particularly sensitive in identifying oedema.
- ICP Monitoring: Invasive technique to measure intracranial pressure directly.
Early and accurate diagnosis is essential for effective management.
Treatment Options
The management of cerebral oedema aims to reduce intracranial pressure and address the underlying cause:
Medical Management
- Osmotherapy: Agents like mannitol and hypertonic saline are used to draw fluid out of the brain tissue. Hypertonic saline has gained popularity due to its effectiveness and lower risk of rebound oedema .
- Hyperventilation: Controlled hyperventilation can lower carbon dioxide levels, leading to vasoconstriction and reduced cerebral blood volume.
- Medications: Antiseizure drugs are administered prophylactically, as patients with cerebral oedema are at high risk for seizures.
Surgical Interventions
- Craniotomy: Surgical removal of part of the skull to allow the brain to expand without being compressed.
- Ventriculostomy: Insertion of a catheter into the ventricles to drain excess cerebrospinal fluid.
- Decompressive Craniectomy: Removal of a portion of the skull to relieve pressure in severe cases.
These interventions are considered when medical management is insufficient.
Prognosis
The outcome of cerebral oedema depends on several factors:
- Severity of Swelling: More extensive oedema often correlates with worse outcomes.
- Timeliness of Treatment: Early intervention can significantly improve prognosis.
- Underlying Cause: Reversible causes generally have a better prognosis.
With prompt and appropriate treatment, many patients recover fully or with minimal deficits.
Prevention
While not all cases of cerebral oedema are preventable, certain measures can reduce risk:
- Prompt treatment of head injuries
- Management of underlying conditions like diabetes and hypertension
- Avoidance of rapid correction of electrolyte imbalances
- Monitoring and managing intracranial pressure in

2 Responses
[…] Introduction […]
[…] Types of Hypertension in Pregnancy […]